Abstract
Introduction: Currently, 37 million people live with HIV. Due to significant advances in HAART, they are living longer compared to previous decades. These patients are at a higher risk of developing hematological malignancies (HM) as compared to general population. Allogeneic hematopoietic stem cell transplantation (Allo-HSCT) is a potentially curative therapy for HM. Many uncertainties exist for HSCT in HIV patients, including optimal donor selection, conditioning regimens, risk for graft-versus-host disease (GVHD) and outcomes.
Methods: For a comprehensive systematic review of literature, we searched PubMed for 'allogeneic stem cell transplant' for 'hematological malignancies' in patients with 'HIV'. After screening, case reports and series, retrospective and prospective studies were included in data collection. The following variables were collected: number of patients, age, HAART, type of donor, stem cell source, conditioning regimen, GVHD prophylaxis, engraftment, infections, GVHD, or other complications, overall survival (OS), and cause of death. Statistical analysis was performed evaluating the risks and outcomes pertaining to the Allo-HSCT. To avoid publication bias, abstracts from annual meetings of professional societies i.e., hematology/HSCT and HIV were screened.
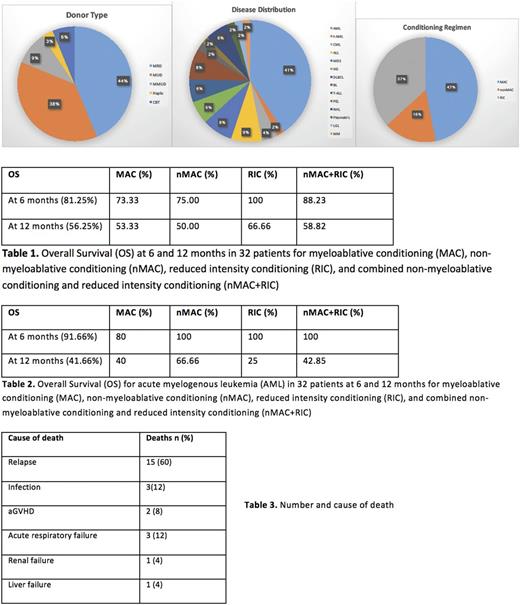
Results: After application of strict selection criteria, 49 patients were included (32 previously reported, and 17 from a recent prospective clinical trial). Forty-six (93.8%) were males. Median age was 34 (17-64) years. Of the 32 patients, 14 (43.7%) received HSCT from matched related donor (MRD), 12 (37.5%) from matched unrelated donor (MUD), 3 (9.4%) from mismatched unrelated donor (MMUD), 1 (3.1%) from haploidentical donor (Haplo), and 2 (6.2%) from cord blood (CBT). Of 49 patients, 21 had AML, including one t-AML. Other cases included CML (2), B- cell ALL (4), MDS (4), Hodgkin's disease (HD, 3), DLBCL (3), Burkitt's lymphoma (BL, 4), T-cell ALL (1), primary effusion lymphoma (PEL, 1), NHL (3), plasmablastic lymphoma (1), large granular leukemia (1), and multiple myeloma (MM, 1). Median CD4 cell count at HSCT was 172 (33-1661). All patients were started or were already on HAART prior to HSCT. Conditioning regimen included myeloablative (MAC) in 23 (47%), reduced intensity (RIC) in 18 (36.7%) and non-myeloablative (non-MAC) in 8 (16.3%) patients. Median time to neutrophil engraftment was 17 (9-48) days. HAART was continued during and after HSCT period with some exceptions. HIV viremia remained undetectable in most of the patients after HSCT with 2 patients requiring alterations in treatment. CMV viremia occurred in 43.7%. Incidence of Grade II-IV GVHD was 41% in recent prospective trial. Acute GVHD (aGVHD) was reported in 19/32 (59.3%) patients, with Grade II in 12 (37.5%), and Grade III in 2 (6.2%). No cases of Grade IV aGVHD were reported. OS at 6, and 12 months was 81.6% and 56.6% respectively for all patients. Among 32 patients, OS at 6 months for MAC was 73.3%, 88.2% for nMAC and RIC combined; OS at 12 months for MAC was 53.3%, 58.8% for nMAC and RIC combined. For AML, OS was 91.6% at 6 months and 41.6% at 12 months. For AML, OS at 6 months with MAC was 80%, 100% for nMAC and RIC combined; OS at 12 months with MAC was 40%, 42.8% for nMAC and RIC combined. Twenty-four patients were alive in CR on long-term follow-up with 25 deaths reported. Fifteen (60%) deaths were from relapse, 3 (12%) from infection, 2 (8%) from GVHD and 5 (20%) from other causes including renal failure, acute respiratory failure and liver failure.
Conclusions: To our knowledge, this is the largest series of "allogeneic" HSCT in HIV patients and its results indicate that clinical outcomes are not significantly different from non-HIV patients (historical control). RIC regimens portray greater likelihood of survival compared to MAC regimens. Likely, the improvements in supportive care, better donor availability and novel conditioning regimens have led to the improvements in survival. Engraftment time is similar to non-HIV patients. Incidence of infections is also comparable. Drug interactions between transplant medications and HAART should be carefully monitored and therapy switched where necessary with involvement of HIV expert. In current era of MRD, MUD, CBT and haplo donors, allo-HSCT remains a feasible therapy for HM in HIV patients, thus the presence of HIV should NOT preclude these patients from this potentially curative therapy when indicated.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.